A new way to visualize single-cell activity in living zebrafish
embryos has allowed scientists to clarify how cells line up in the right
place at the right time to receive signals about the next phase of
their life.
 |
Under normal circumstances in zebrafish embryos, cells oscillate in synchrony
with their neighbors as they prepare to make segments that later become
muscle and vertebrae. When a color map (top left corner) is used to indicate the
phase of oscillation in each cell at any fixed snapshot of time, with cool colors
representing the peak of the gene activation wave and warm colors the lower
levels of activation, it is evident in the top image that neighboring cells are in a
similar phase, or transitioning smoothly to the next phase. However, in embryos
lacking a powerful messaging system called Notch signaling, that synchrony is
lost. In the bottom map, cells in mutant embryos that lack the Notch signal are
oscillating, but the random assortment of colors without smooth transitions
shows that Notch is required to synchronize the oscillations in neighboring cells.
Images courtesy of Ohio State University |
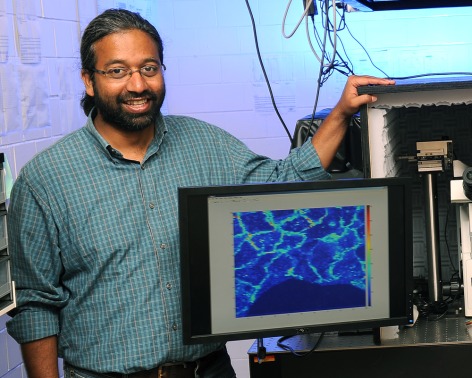
Scientists developed the imaging tool in single living cells by
fusing a protein defining the cells’ cyclical behavior to a yellow
fluorescent protein that allows for visualization. Zebrafish embryos are
already transparent, but with this closer microscopic look at the
earliest stages of life, the researchers have answered two long-standing
questions about how cells cooperate to form embryonic segments that
later become muscle and vertebrae.
Though these scientists are looking at the molecular “clock”
that defines the timing of embryonic segmentation, the findings increase
understanding of cyclical behaviors in all types of cells at many
developmental stages – including problem cells that cause cancer and
other diseases. Understanding how to manipulate these clocks or the
signals that control them could lead to new ways to treat certain human
conditions, researchers say.
Embryonic cells go through oscillating cycles of high and low
signal reception in the process of making segmented tissue, and gene
activation by the groups of cells must remain synchronized for the
segments to form properly. One of a handful of powerful messaging
systems in all vertebrates is called the
Notch signaling pathway, and its precise role in this oscillation and synchronization has been a mystery until now.
In this study, the researchers confirmed that the cells must receive
the Notch signal to maintain synchronization with nearby cells and form
segments that will become tissue, but the cells can activate their genes
in oscillating patterns with or without the signal.
“For the first time, this nails it,” said
Sharon Amacher, professor of
molecular genetics at Ohio State University
and lead author of the study. “This provides the data that cells with
disabled Notch signaling can oscillate just fine, but what they can’t do
is synchronize with their neighbors.”
The imaging also allowed Amacher and colleagues to determine
that cell division, called mitosis, is not a random event as was once
believed. Instead, division tends to occur when neighboring cells are at
a low point of gene activation for signal reception – suggesting
mitosis is not as “noisy,” or potentially disruptive, as it was
previously assumed.
The study is published in the November issue of the journal
Developmental Cell.
Amacher’s work focuses on the creation of these tissue segments, called
somites, in the
mesoderm of zebrafish embryos – this region gives rise to the ribs, vertebrae and muscle in all vertebrates, including humans.
“This early process of segmentation is really important for
patterning a lot of subsequent developmental events – the patterning of
the nervous system and the vasculature, much of that depends on this
clock ensuring that early development happens properly,” Amacher said.
Unlike the well-known 24-hour Circadian clock, however, the
activities of cells at the earliest stages of development can occur
within a matter of minutes – which makes their clocks very challenging
to study.
Experts in tissue segmentation liken the oscillating cycle of gene
activation and de-activation that cells go through before they form
somites to the wave that fans perform in a stadium. According to the
segmentation clock, genes are turned on, proteins are made, proteins
then inhibit gene activation, and so on, and the pattern repeats until
all necessary somites are formed. Neighbor cells must be in sync with
each other just as sports fans in the same section must stand and sit at
the same time to effectively form a wave.
Zebrafish somites form every 30 minutes, meaning that during
any one cycle of the wave, a cell is engaged in making protein for only
about five minutes. To generate the imaging tool, researchers linked a
yellow fluorescent protein to a cyclic protein known to have a short
lifespan. The resulting short-lived fluorescent fusion protein allowed
Amacher and colleagues to look at single cells along with their
neighbors to observe how they stayed synchronized as they did the wave.
Researchers in this field had previously thought that the Notch
signaling pathway may be needed to start the clock in these cyclic
genes, though conflicting data had shown that the clock could run
without the signal.
Amacher’s imaging showed that, indeed, Notch was required only
to maintain synchronization, but not to start the oscillating clock. She
and colleagues tested this idea by combining the imaging tool with
three mutant cell types with disabled Notch signals. Cells in all three
mutants could oscillate, but not in a synchronized fashion, explaining
how they failed to form segments in the way that cells receiving the
Notch signal could.
Defects in Notch signaling are associated with human congenital
developmental disorders characterized by malformed ribs and vertebrae,
suggesting this work offers insight into potential therapies to prevent
these defects.
The researchers next sought to determine whether cell division
interrupted the synchrony needed for creation of the segments. Mitosis,
occurring among 10 to 15 percent of embryonic cells at any one time, is
considered a source of biological “noise” because when cells divide,
they stop activating genes. If division were happening randomly, as
previously thought, instead of in a pattern, the very cell division
needed for organism growth could also disrupt clock synchrony, creating
problems that segmenting organisms would have to overcome.
The study showed, however, that most cells divided when their
neighbors were at a low point of gene activation – at the bottom of a
wave – suggesting that cell division doesn’t occur at random. The study
team noted that the two daughter cells created from a fresh division are
more tightly synchronized with each other than are any other cell
neighbors in the area.
Under normal conditions, these two daughters resynchronize with
their neighbors in short order. In embryos lacking Notch signaling,
newly divided daughters appeared as a pair of tightly synchronous cells
in a largely asynchronous sea, showing that oscillation could resume
without the signaling pathway. Without Notch, the daughter cells
gradually drifted out of synchrony, becoming like their asynchronous
neighbors.
Amacher said these findings could be incorporated into models
of developmental cell behavior to further advance cell biology research.
“Most of our tissues and organs are not made up of the same
types of cells. They have different jobs. So you don’t want them to
respond identically to every signal; you want them to have different
responses,” she said. “We need to understand systems like this that help
cells not only interpret the signals in their environment, but do the
right thing when they get that signal.”
source:http://researchnews.osu.edu/archive/cellclock.htm